Recently, a good friend consulted me for advice on pre-op antibiotics for her upcoming hernia operation. Her surgeons were pushing for a broad spectrum cephalosporin ‘just in case’ to suppress any potential infection. I pushed back, knowing the risks with using prophylactic antibiotics in hospitalized elderly patients often outways the potential benefit. My biggest concern is C. Diff.
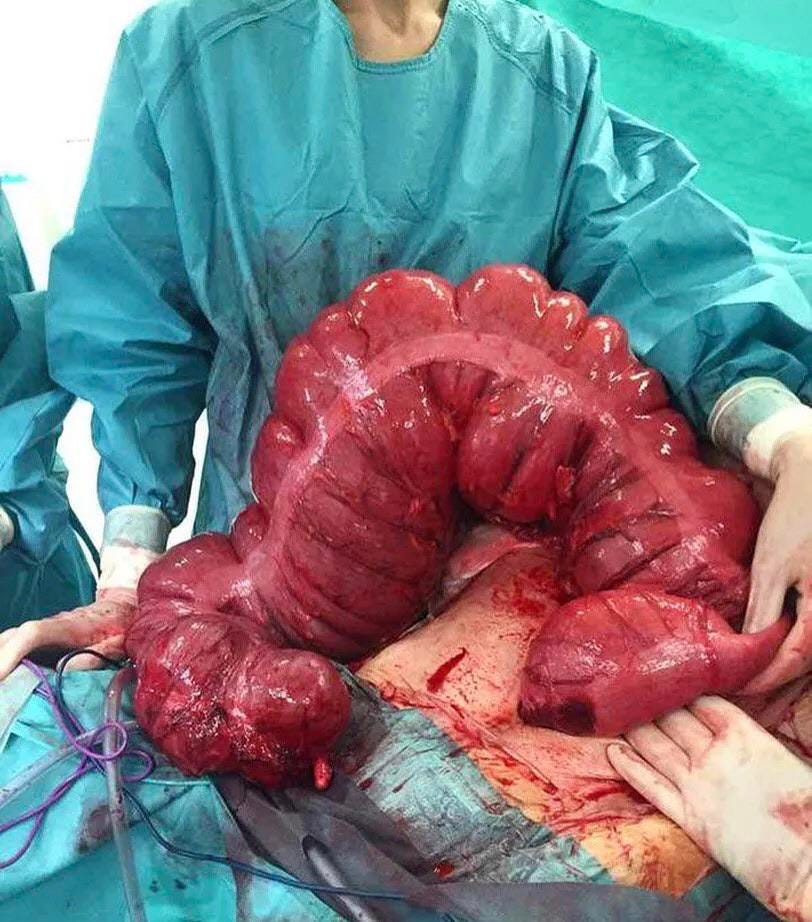
Clostridioides difficile, often referred to as C. difficile or C. diff, is a bacterium that causes severe intestinal illness. It is a gram positive, anaerobic, spore forming bacterium spread by the fecal oral route. It produces toxins A and B, causing severe mucosal destruction and pseudomembrane formation. Approximately 1 in 6 patients infected with C. difficile will be reinfected within two months. Toxic megacolon is a severe complication of Clostridium difficile colitis. About 15,000 to 30,000 die from infection with the C. diff bacteria in the United States each year.
As you can see, my concerns are legit.
CDC Fact Sheet:
Risk Factors:
Risk factors for development of toxic megacolon include concurrent malignancy, severe chronic obstructive pulmonary disease, organ transplantation, cardiothoracic procedures, diabetes mellitus, immuno suppression and renal failure.
The most important modifiable risk factor for the development of CDI is exposure to antibiotic agents. Clindamycin, third-/fourth-generation cephalosporins, carbapenems, and fluoroquinolones are the most common antibiotics associated with C. difficile infection. Even very limited exposure, such as single-dose surgical antibiotic prophylaxis, increases a patient’s risk of C. difficile colonization and symptomatic disease.
Infants and children who are given prescription acid-reducing medications face a substantially higher risk of developing Clostridium difficile infection. Pediatricians are advised against prescribing these drugs for children who have non-specific gastrointestinal symptoms such as occasional vomiting.
The study found that 2.6% (17 of 650) of the children diagnosed with C. diff. infection had used PPIs/H2RAs within 90 days, compared with just 0.3% (8 of 3,200) of the controls. In other words, use of acid-reducing drugs resulted in a seven-fold increase in risk for infection with C. diff. The effect was stronger for PPIs, which are more powerful than H2RAs. [histamine-2 receptor antagonists]
The researchers suspect that, like antibiotics, acid reducing medications may increase the risk of C. diff. infection by altering the gastrointestinal microbiome. - https://medicalxpress.com/news/2015-06-acid-reducing-medications-sharply-diff-bacteria.html
Another potential risk factor may come from excesses in dietary zinc. This is a real concern given the ‘immune supplements’ that dose large amounts of the metal ion.
Excess dietary zinc (Zn) substantially alters the gut microbiota and, in turn, reduces the minimum amount of antibiotics needed to confer susceptibility to CDI. In mice colonized with C. difficile, excess dietary Zn severely exacerbated C. difficile–associated disease by increasing toxin activity and altering the host immune response. In addition, we show that the Zn-binding S100 protein calprotectin has antimicrobial effects against C. difficile and is an essential component of the innate immune response to CDI. Taken together, these data suggest that nutrient Zn levels have a key role in determining susceptibility to CDI and severity of disease, and that calprotectin-mediated metal limitation is an important factor in the host immune response to C. difficile. - J Moore et al.
TREATMENTS
The medical management of toxic megacolon includes, bowel rest, bowel decompression, and replacement of fluids and electrolytes. Stop medications that slow intestinal motility, such as, anticholinergics, antidepressants, antidiarrheals, and narcotics.
Antibiotics:
Oral vancomycin, IV metronidazole, vancomycin 500 mg enemas every 12 hr.
Probiotic Foods:
Anticipating the altered microbiome, many docs push probiotics when giving antibiotics. These foods include items such as sauerkraut, yogurt, miso, and kimchi.
Hospitalized adult patients on antibiotics who were also given probiotics had a lower incidence of C. diff infection than controls (1.6% vs. 3.9%). For every day in delay giving the probiotic in relationship to the first antibiotic dose, there is a significant decrement in efficacy.
Soluble fiber foods that form a slurry are also helpful. These include items such as rice congee, pumpkin soup, and applesauce,
Fecal Transplant:
FDA just approved the biologic product, Ferring Pharmaceuticals Rebyota, as the first live microbiome-based therapeutic for the prevention of recurrent Clostridioides difficile infection (CDI) and works by restoring the functionality of a patient’s microbiome after antibiotic treatment. It is prepared from human stool samples that are tested for a range of transmissible pathogens. The treatment is administered rectally in one dose.
The approval was based on two randomized, double-blind clinical studies and some open label clinical studies, involving a total of 978 adults. Combining all results, the overall success rate in preventing recurrent CDI for eight weeks was 70.6% in the Rebyota group and 57.5% in the placebo group.
~~~~~~~~~~
Now that the FDA has opened the door to live microbiome-based therapeutics, I suspect we will also see approvals for other indications, such as Multiple Sclerosis and inflammatory bowel diseases.
REFERENCES
Sayedy L, Kothari D, Richards RJ. Toxic megacolon associated Clostridium difficile colitis. World J Gastrointest Endosc 2010; 2(8): 293-297 http://www.wjg-net.com/1948-5190/full/v2/i8/293.htm DOI: http://dx.doi.org/10.4253/wjge.v2.i8.293
Acid-reducing medications sharply raise risk of C. diff. bacteria infection in kids (2015, June 17) https://medicalxpress.com/news/2015-06-acid-reducing-medications-sharply-diff-bacteria.html
J Moore et al. Dietary zinc alters the microbiota and decreases resistance to Clostridium difficile infection, Nature Medicine, DOI: 10.1038/nm.4174
P Maguire. Timing is everything in preventing C. diff. Patients should take probiotics within two days of an antibiotic dose. June 2017 https://www.todayshospitalist.com/timing-is-everything-in-preventing-c-diff/
First FDA-approved fecal-based treatment helps fight a tough superbug (2022, December 1) https://medicalxpress.com/news/2022-12-fda- approved-fecal-based-treatment-tough-superbug.html
https://www.fda.gov/vaccines-blood-biologics/vaccines/rebyota






In addition, aren’t there additional risks when taking fluoroquinolones like ligament damage? What do you think?
Excellent article. As one who acquired C Diff after many antibiotics for a sepsis event, I can say that it often returned with a vengeance over a rather long time. I became good friends with Flagyl and its consequences. I can detect the odor of the toxins immediately, no culture required. Only bleach and alcohol along with soapy cloths are useful in eliminating spores, nasty creatures.
For a time I worried about needing those advanced antibiotics and discussed a fecal transplant from a healthy donor. Not easy to get a transplant approved partly because of the testing needed, many of us carry the spores held in check buy good bacteria. I did find Florastore helpful in getting my gut back.
I can say I've been fairly lucky in getting control back. There are some who do end up in very bad condition fighting C Diff. Not sure why some suffer much more than others. I suppose a healthy gut has a lot to do with it.