I started out January with the brain as topic, so let’s keep it rolling along.
My previous newsletters discussing aromatase and puberty mentioned estradiol synthesis in the brain from testosterone precursors; now we extend it to talk about its role in healing brain injuries.
TRAUMA
The female gonadal steroid may be life-saving on the battlefield, where war injury deaths result from blood loss. In experiments, it prolonged survival in the face of massive loss of blood. Estradiol (E2) allowed survival for three hours without fluid resuscitation, and long-term survival if fluid resuscitation was provided after 3 hours. Blood loss shock and consequential tissue hypoxia affects mitochondrial function, endoplasmic reticulum stress markers and inflammatory cytokine production, and E2 mitigated those changes. Chaudry et al first used microencapsulated cyclodextrin E2, then developed a synthetic estrogen, ethinyl estradiol-3-sulfate (EE-3-SO4) which could be carried in a small autoinjector for use. Treatment resulted in 6-hour survival rates of 50 to 80 percent in porcine and murine experimental models respectively. EE-3-SO4 dilates blood vessels and thus reduces third spacing, increasing blood volume, improving heart performance, heart output and liver function. E2 also attenuates increases in interleukin-6, a pro-inflammatory cytokine.
These results were the proof of principle basis for initiating clinical studies in soldiers and domestic trauma patients. EE-3-SO4 may also be a treatment after traumatic brain injury. Experiments, show that the estrogen reduces cerebral edema, increases brain blood flow, increases cognitive function and memory, and lessens brain cell death.
Joshua Gatson showed that estrone reduces inflammation and cell death after traumatic brain injury. The study in male rats, compared 0.5 mg of estrone to a placebo, dosed 30 minutes after the injury. Estrone promoted brain-derived neurotrophic factor (BDNF), which inceased cell survival.
Aromatase, the enzyme that converts testosterone to estrogen, has big role in the healthy, and injured brain.
… there's mounting evidence that in the healthy brain, aromatase and the estrogen it enables neurons to produce, helps keep our brains and us nimble. Now scientists are learning that with injury, aromatase and estrogen expression seem to shift to cells in the brain called astrocytes, aiding their support and nurturing of now-stressed neurons, …
Even in culture, neurons will connect and communicate, but when scientists add an aromatase inhibitor to the mix, connectivity is interrupted. Some of the first in vivo studies in zebra finches showed that aromatase levels increased following a brain injury, which also supports a protective role for the protein. More brain damage results when aromatase inhibitors are given. "There seemed to be more inflammation," - Dr. Darrell Brann, Medical College of Georgia, 2015
INFLAMMATION
In studies of zebra finches Pedersen et al found that estrogen-producing glial cells play a role in the rapid response to brain injury. The inflammation control happened within hours. In exploring how hormones communicate with neurons, they discovered a new method of communication, synaptocrine signaling, by which neurons create and feed high levels of estrogen to one another.
In the first experiment, researchers injured both sides of the brain, but only one side received an estrogen dose. The treated side had less inflammation. They controlled the endogenous levels of estrogen by inhibiting aromatase. In a second experiment, researchers injured both sides of the songbird brain but limited aromatase function to only one side of the brain. On the side without aromatase, the inflammatory cytokines remained elevated.
HYPOXIA
There is a beneficial role of neuron-derived E2 in astrocyte activation, neuroprotection and cognitive preservation following ischemic injury to the brain. Yujiao Lu et al experimented with a forebrain neuron-specific aromatase knockout (FBN-ARO-KO) mouse model and used it to deplete neuron-derived E2 in the forebrain in order to determine its roles after global cerebral ischemia (GCI). Ovariectomized female FBN-ARO-KO mice had less astrocyte activation, attenuated astrocytic aromatization and decreased hippocampal E2 levels. FBN-ARO-KO mice exacerbated neuronal damage and cognitive dysfunction after GCI. Intact male mice showed similar results.
ESTRADIOL POLYMERS
So 17β-estradiol (E2) targets and induces beneficial phenotypic changes within the CNS cells following injury.
AR D’Amato et al. addressed the need for prolonged E2 release, and generated poly(pro-E2) biomaterial scaffolds that can release E2 in vitro at nanomolar concentrations, for 1–10 years, via a slow hydrolysis. The scaffolds promote and guide neurite extension ex vivo, and protect neurons from oxidative stress in vitro. Their properties demonstrate next-generation implantable biomaterials with prolonged release and excellent regenerative potential.
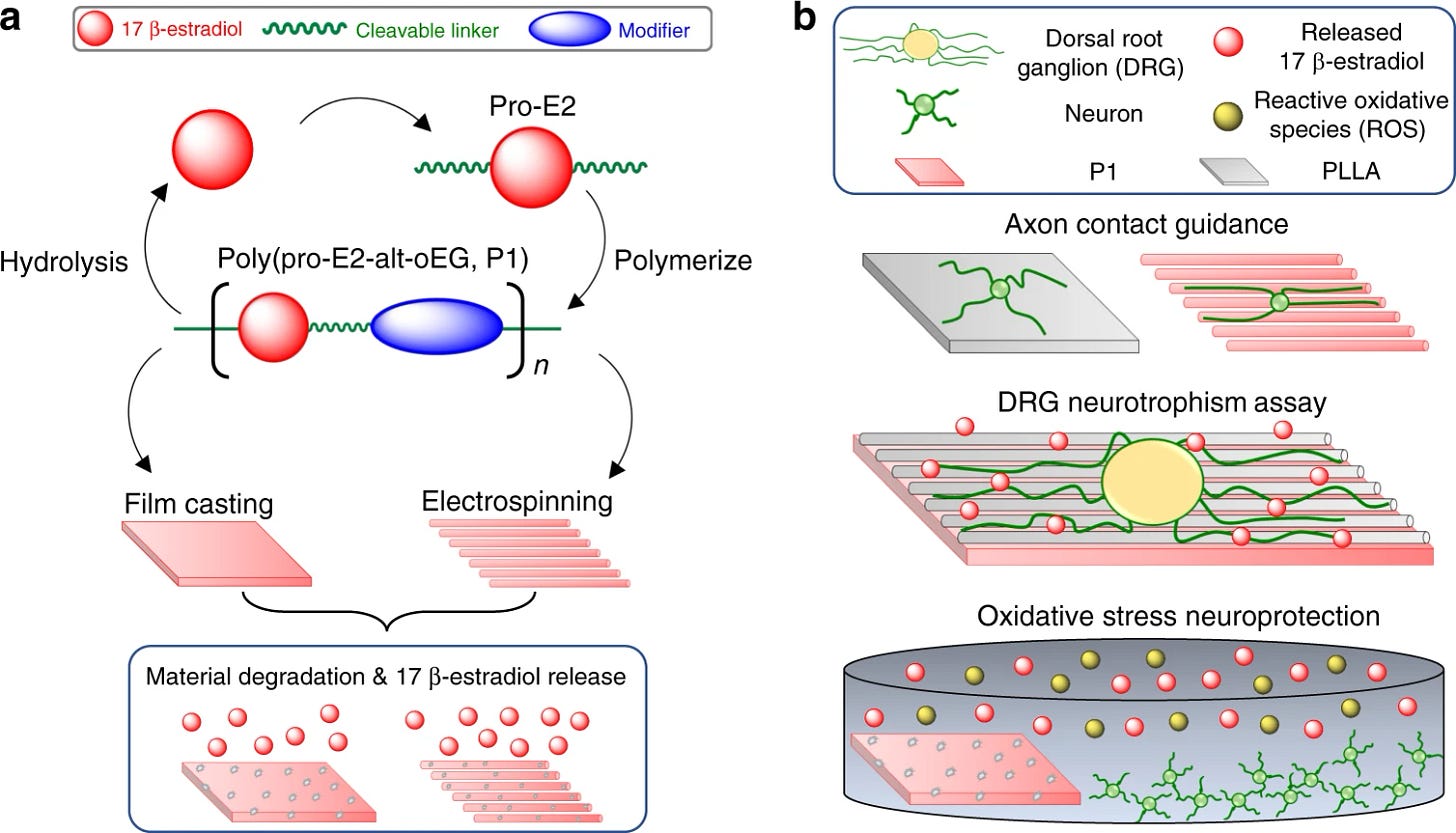
17β-Estradiol (E2) confers neuroprotection in preclinical models of spinal cord injury when administered systemically. But can the result also occur if E2 was applied locally to the injured spinal cord for a sustained duration using poly(pro-E2) film biomaterials? Following contusive spinal cord injury in adult male mice, MK Gottipati et al subdurally implanted poly(pro-E2) films then assessed neuroprotection 7 days after injury. The poly(pro-E2) films modestly improved neuroprotection, but did not affect the inflammatory response, when compared to the injured controls.
So exciting to see the many potential applications of estrogen for these grave indications. And each study helps to suss out the mechanisms of action for neuroprotection, leading to more promising therapeutic candidates.
Hope to soon see these TBI treatments being used in active practice at the bedside. Translational Medicine at its best.
REFERENCES
Chaudry, et al. Female sex hormone may save injured soldiers on the battlefield (2015, November 2) https://medicalxpress.com/news/2015-11-female-sex-hormone-soldiers- battlefield.html
Joshua Gatson. Estrogen hormone reveals protective ability after traumatic brain injury (2012, April 23) https:/medicalxpress.com/news/2012-04-estrogen-hormone-reveals-ability-traumatic.html
Darrell Brann. Enzyme that converts testosterone to estrogen has big role in the healthy, injured brain https://medicalxpress.com/news/2015-05-enzyme-testosterone-estrogen-big-role.html
AL Pedersen, et al. Centrally Synthesized Estradiol Is a Potent Anti-Inflammatory in the Injured Zebra Finch Brain Endocrinology, Volume 157, Issue 5, 1 May 2016, Pages 2041–2051, https://doi.org/10.1210/en.2015-1991
Yujiao Lu, et al. Neuron-Derived Estrogen is Critical for Astrocyte Activation and Neuroprotection of the Ischemic Brain, The Journal of Neuroscience (2020). DOI: 10.1523/JNEUROSCI.0115-20.2020
AR D’Amato, et al. Vastly extended drug release from poly(pro-17β-estradiol) materials facilitates in vitro neurotrophism and neuroprotection NATURE COMMUNICATIONS | (2019)10:4830 https://doi.org/10.1038/s41467-019-12835-w
MK Gottipati et al. Acute Dose-Dependent Neuroprotective Effects of Poly(pro-17β-estradiol) in a Mouse Model of Spinal Contusion Injury, ACS Chemical Neuroscience (2021). DOI: 10.1021/acschemneuro.0c00798







Ngan Pan Bennett Au et al,
Low-dose ionizing radiation promotes motor recovery and brain rewiring by resolving inflammatory response after brain injury and stroke, Brain, Behavior, and Immunity (2023).
DOI: 10.1016/j.bbi.2023.09.015