Diseases of autoimmunity - when body attacks self - are certainly current topics in media, news and medicine. Scientific discussion of vaccine development demands that safety be high priority and adverse autoimmune reactions are top on the surveillance radar monitors.
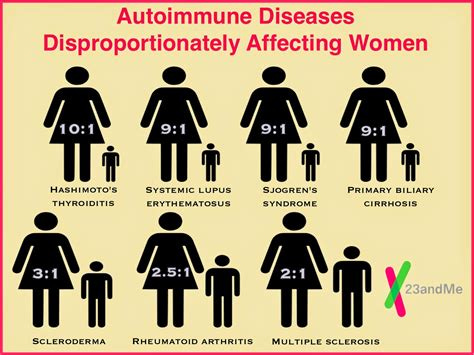
And long known to docs worldwide is that most of those afflicted are and will be women. This observation has persisted for generations, so naturally, the question arises - what is it about femaleness that brings on the raised risk?
All organs and tissues are involved, including brain. So any proposed mechanisms of action must explain the pervasive nature of effect.
Three hypotheses have gained traction. One involves female chromosomes and the other two relate to females being ‘birthing persons.’
Inactivated X Chromosome Activation
After an egg is fertilized by sperm, if there are two X chromosomes - a girl baby - only one chromosome per cell is ‘allowed’ to be active. The other one is ‘silenced’ and gene expression from it is suppressed (the female-specific mechanism for dosage compensation). However, this regulatory process requires energy. In lymphocytes, the inactive X chromosome is predisposed to become partially reactivated and thus result in the overexpression of immunity-related genes. [Most of the immune response genes are packed into that chromosome].
Lymphocytes from female systemic lupus erythematosus patients have different epigenetic characteristics on the inactive X that hinders transcriptional silencing. Instead of tight knot of closed heterochromatin, it seems broken into pieces and scattered across the nucleus; evidence of biallelic expression of immunity-related genes, and increased transcription of these genes.
Immune Overcompensation for Pregnancy Suppression?
Another theory puts the focus on the placenta and the foreign fetal tissue invasion of it. Female immune systems have to dial down when nurturing a fetus for nine months. But the body still must fight off the usual pathogens or will not survive to birth the babe. So sex-specific immune modulation evolved to facilitate survival in this predicament; gene content and dosage on the X chromosomes, being regulated by gonadal and placental hormones.
During pregnancy, the placenta generates huge amounts of estrogens, estriol being the most prevalent. Many autoimmune diseases ‘calm down’ during pregnancy episodes and these steroids are thought to be the drivers to dial back the flares. Recent clinical trials used estriol as therapy for Multiple Sclerosis patients with good results - even for the male patients.
Microchimerism
Did you know that females carry many generations of foreign fetal DNA? Mothers accumulate their own children's cells, but also their own mother's cells and all the cells from the siblings born before her, and maybe even from the maternal grandmother. These fetal cells last life long and show up everywhere in the body, including the brain.
Microchimerism is the presence of cells from one individual in another genetically distinct individual. Pregnancy is the main cause of natural microchimerism through transplacental bi-directional cell trafficking between mother and fetus. In addition to a variety of cell-free substances, it is now well-recognized that some cells are also exchanged in pregnancy. Furthermore, it is now known that microchimerism persists decades later both in mother and in her progeny. The consequences of pregnancy-related microchimerism are under active investigation. However, many authors have suggested a close relationship linking fetal microchimerism and the development of autoimmune diseases. - S Shrivastava et al.
What about women who are never pregnant? Have no blood transfusions, organ transplants, no womb siblings. How does foreign DNA incorporate into them? It can come from maternal sources that intermix in the placenta, as explained before. But… maybe it is DNA from a sex partner’s semen? The possibility does exist, but if it does happen, it is a rare event. Fetal cells can get away with floating around a woman’s body because they lack immune identity [stemcell-like], and do not trigger a foreign body immune backlash. But semen does. And the vagina launches a vigorous reaction. Actually, one known cause of infertility is the female’s “allergy” to her partner’s ejaculate.
Ah yes, we gals can be very picky about with which multiple ‘persons’ we will cohabitate.
REFERENCES
XJ Wanga, et al Unusual maintenance of X chromosome inactivation predisposes female lymphocytes for increased expression from the inactive. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4833277/pdf/pnas.201520113.pdf
H Natri et al. The Pregnancy Pickle: Evolved Immune Compensation Due to Pregnancy Underlies Sex Differences in Human Diseases https://doi.org/10.1016/j.tig.2019.04.008
We are multitudes https://aeon.co/essays/microchimerism-how-pregnancy-changes-the-mothers-very-dna
S Shrivastava et al. Microchimerism: A new concept https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6714269/
AJ Crean. Revisiting telegony: offspring inherit an acquired characteristic of their mother's previous mate. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4282758/
Please subscribe to my free newsletter by clicking the button. Many future stories will be exclusive to only paid subscribers to BioMedWorks Newsletter: the PREMIUM CONTENT. I would be grateful if you do go on to upgrade to the paid subscription for just $5 a month or $50 a year.








Tzu-Yu Shao et al, Reproductive outcomes after pregnancy-induced displacement of preexisting microchimeric cells, Science (2023).
DOI: 10.1126/science.adf9325.
www.science.org/doi/10.1126/science.adf9325
Presence of fetal cells in women lowers risk of breast cancer but raises risk of colon cancer
https://medicalxpress.com/news/2012-05-presence-fetal-cells-women-lowers.html