"When the well is dry, we know the worth of water."- Benjamin Franklin
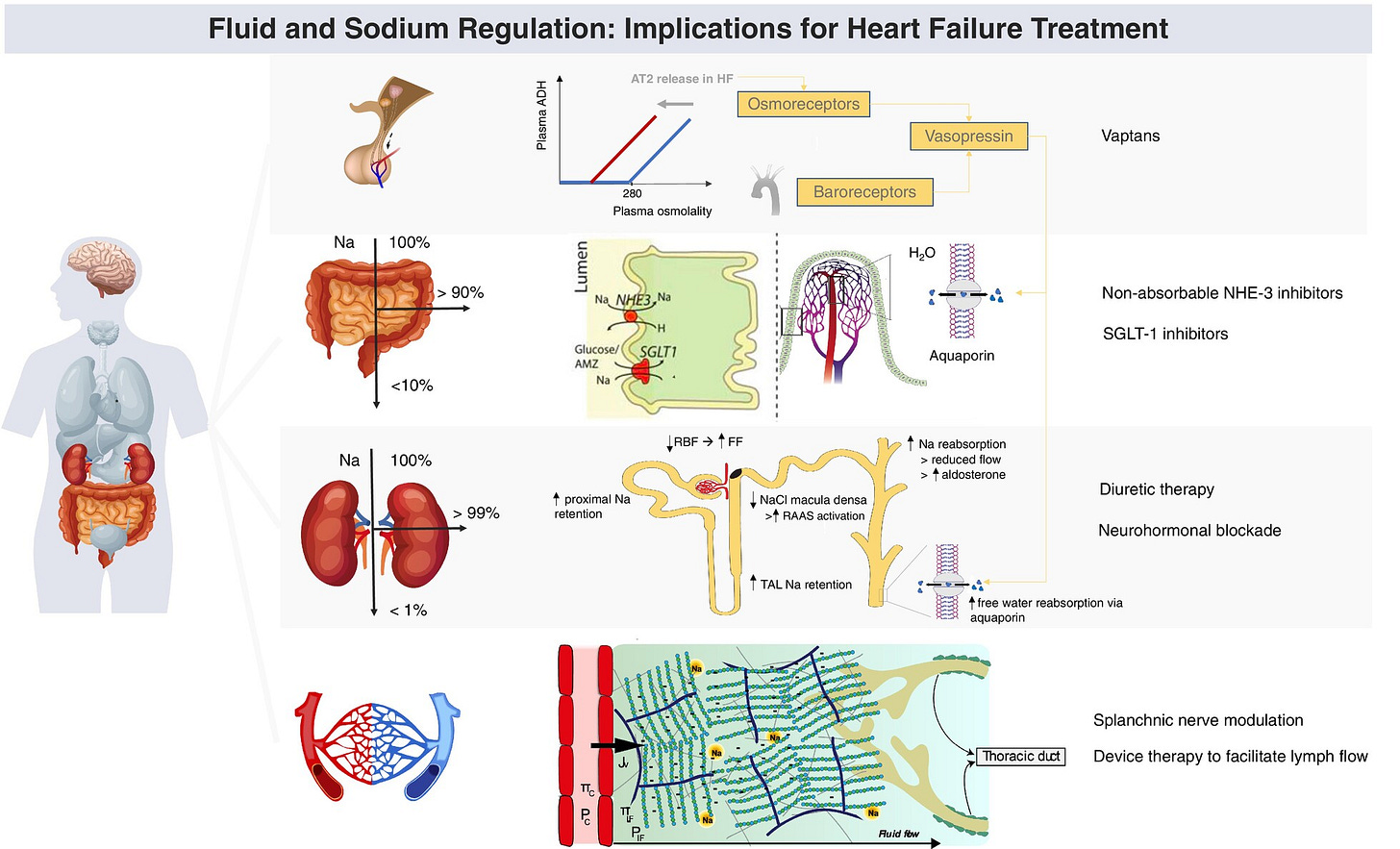
My past newsletter reported on the successful use of a diabetes drug to treat heart failure: SGLT2i, improves solute excretion without loss of free water.
Sodium Glucose Co-Transporter 2 inhibitors (SGLT2i): not just for diabetes
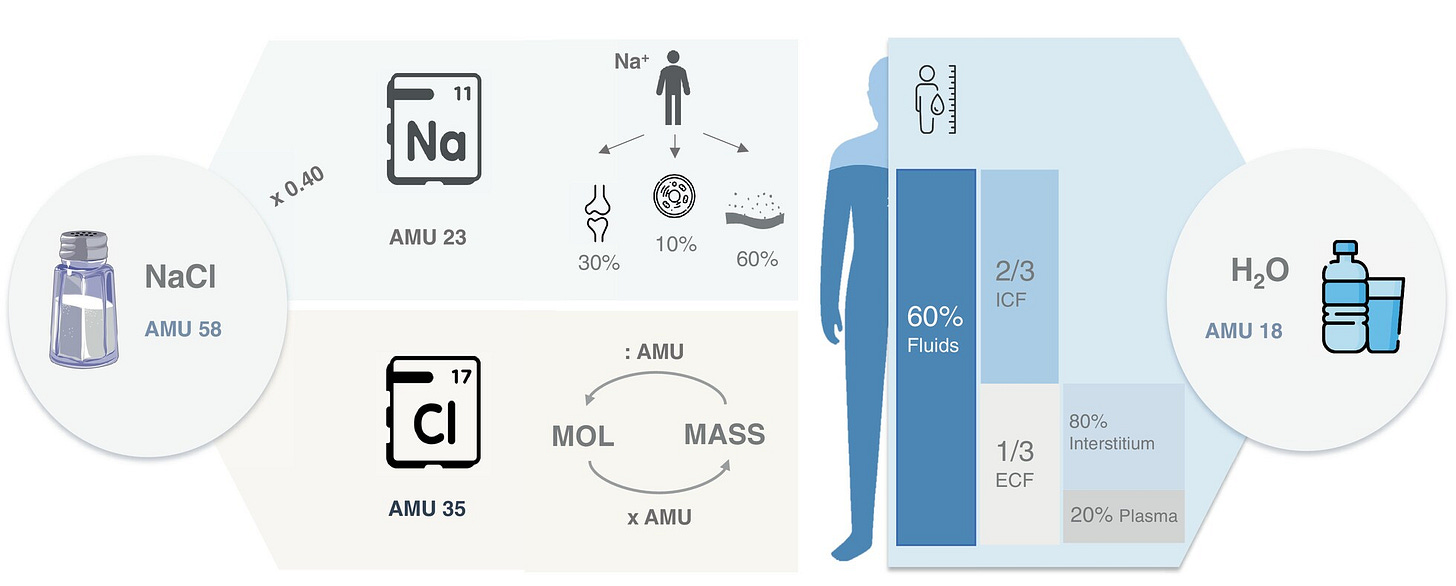
Sodium-glucose co-transporter-2 (SGLT-2) inhibitors are antihyperglycemic agents acting on the SGLT-2 proteins expressed in the proximal convoluted tubules. These drugs exert their effect by preventing the reabsorption of filtered glucose from the tubular lumen.
This report extends the water news on CHF treatments to recommend liberalizing fluid management.
CHF treatments
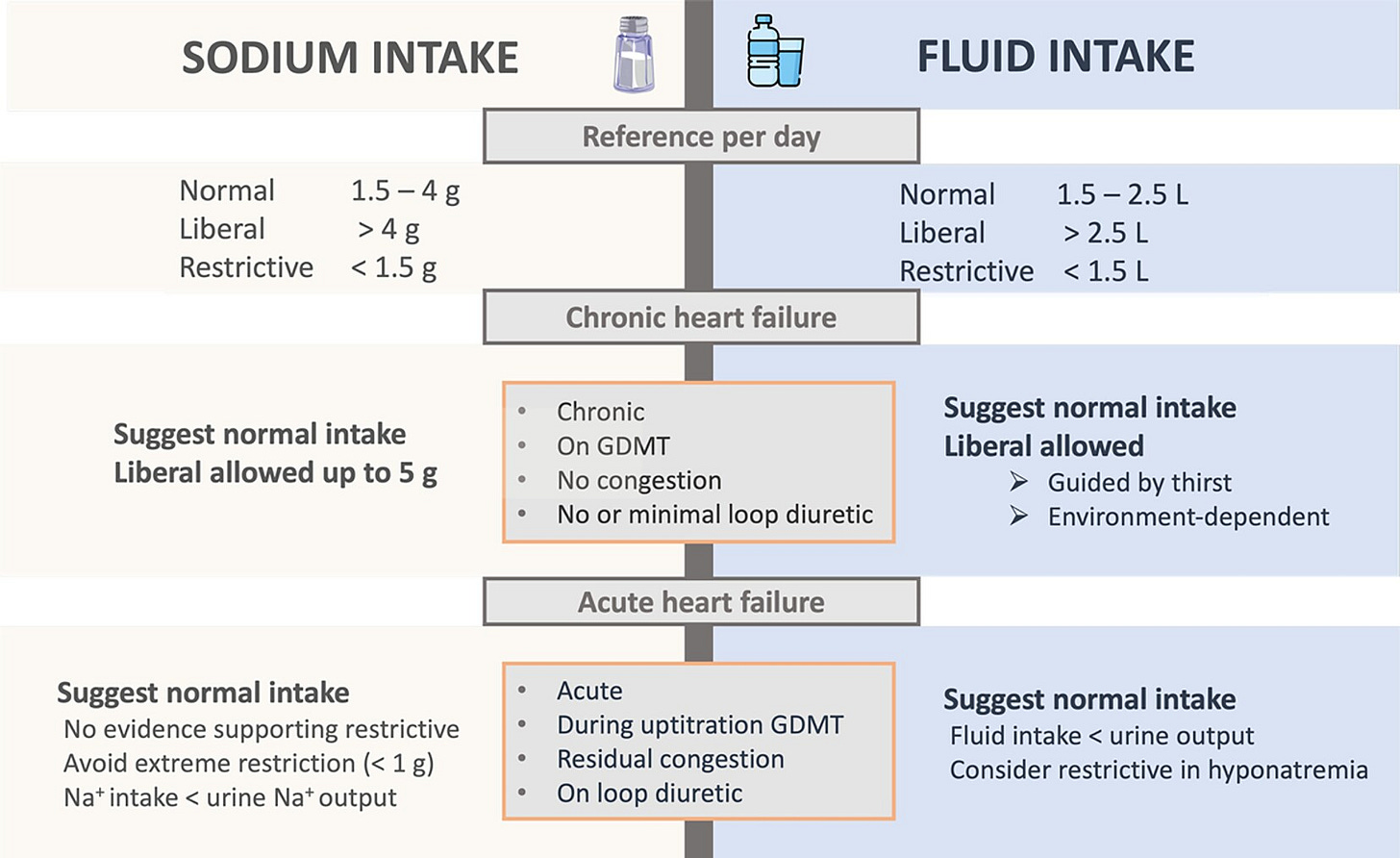
In heart failure, the body increases left ventricular filling volume/pressure to compensate for the decrease in the heart’s force of contraction. This leads to pulmonary congestion and peripheral edema. Traditional therapies target sodium and fluid intake, restricting them.
However, thirst complaints occur in 50% of acute HF patients under retricted fluid intake, impacting their quality of life — xerostomia, altered taste, dry skin and itching are suffered side effects.
A recent clinical trial examined the question: would stable CHF patients be negatively impacted if they were allowed to freely regulate their own fluid intake according to their own needs. Results showed that whether or not these patients followed a restricted fluid intake, there were no differences in their health status, hospital admissions, mortality, or medication use. Those without restrictions only consumed about 300 milliliters more daily — the equivalent of two cups of coffee. The single significant finding was that those with restricted fluid intake experienced more symptoms of thirst.
Thus, drinking less is unnecessary for stable heart failure patients.
Fluid restriction is frequently recommended to patients with chronic heart failure, but randomized clinical trials assessing the effects of fluid restriction remain scarce. In this multicenter open-label trial, outpatients with chronic heart failure were randomized to receiving advice for liberal fluid intake versus receiving advice for fluid restriction, up to 1,500 ml per day of fluid intake. The primary outcome of the trial was health status after 3 months, as assessed by the Kansas City Cardiomyopathy Questionnaire Overall Summary Score (KCCQ-OSS). Secondary outcomes included thirst distress and safety events. Among 504 randomized patients (67.3% male), the KCCQ-OSS after 3 months was 74.0 in the liberal fluid intake group versus 72.2 in the fluid restriction group, with a mean difference after adjustment for baseline scores of 2.17 (95% confidence interval −0.06 to 4.39; P = 0.06), indicating that the primary outcome was not met. Thirst distress was higher in the fluid restriction group and no differences were observed for safety events between the two groups. These findings question the benefit of fluid restriction in chronic heart failure. ClinicalTrials.gov registration: NCT04551729.
The European Society of Cardiology HF guidelines downgraded their recommendations over time, and currently advise for the limitation of salt intake to no more than 5 g/day in patients with HF, while contemplating fluid restriction of 1.5–2 L/day only in selected patients.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
"Water is life’s matter and matrix, mother and medium. There is no life without water." — Albert Szent-Györgyi
REFERENCES
W Mullens, et al. Dietary sodium and fluid intake in heart failure. A clinical consensus statement of the Heart Failure Association of the ESC. Eur J Heart Fail. 2024 Apr;26(4):730-741. doi: 10.1002/ejhf.3244. Epub 2024 Apr 12. https://onlinelibrary.wiley.com/doi/10.1002/ejhf.3244
JJ Herrmann, et al. Liberal fluid intake versus fluid restriction in chronic heart failure: a randomized clinical trial. Nat Med (2025). https://doi.org/10.1038/s41591-025-03628-4