Girl gonadal steroids stimulate Tcells to titrate opioid peptides
estrogen and progesterone take pain away
In a past newsletter, I reported on estrogen’s ability to heal brain injuries.
Estrogen helps heal Traumatic Brain Injury
I started out January with the brain as topic, so let’s keep it rolling along.
One area of focus was inflammation that was controlled by the glial cells.
“INFLAMMATION
In studies of zebra finches Pedersen et al found that estrogen-producing glial cells play a role in the rapid response to brain injury. The inflammation control happened within hours. In exploring how hormones communicate with neurons, they discovered a new method of communication, synaptocrine signaling, by which neurons create and feed high levels of estrogen to one another.
In the first experiment, researchers injured both sides of the brain, but only one side received an estrogen dose. The treated side had less inflammation. They controlled the endogenous levels of estrogen by inhibiting aromatase. In a second experiment, researchers injured both sides of the songbird brain but limited aromatase function to only one side of the brain. On the side without aromatase, the inflammatory cytokines remained elevated.”
Hence, E2 synthesis (via aromatase) after brain injury is a potent and inducible anti-inflammatory signal, with specific modulation of discrete cytokine signaling.
Now a recent study reports a sex-dependent influence on these brain cells —they are driven by estrogen and progesterone. Female hormones can stimulate immune cells to make opioids that can suppress pain.
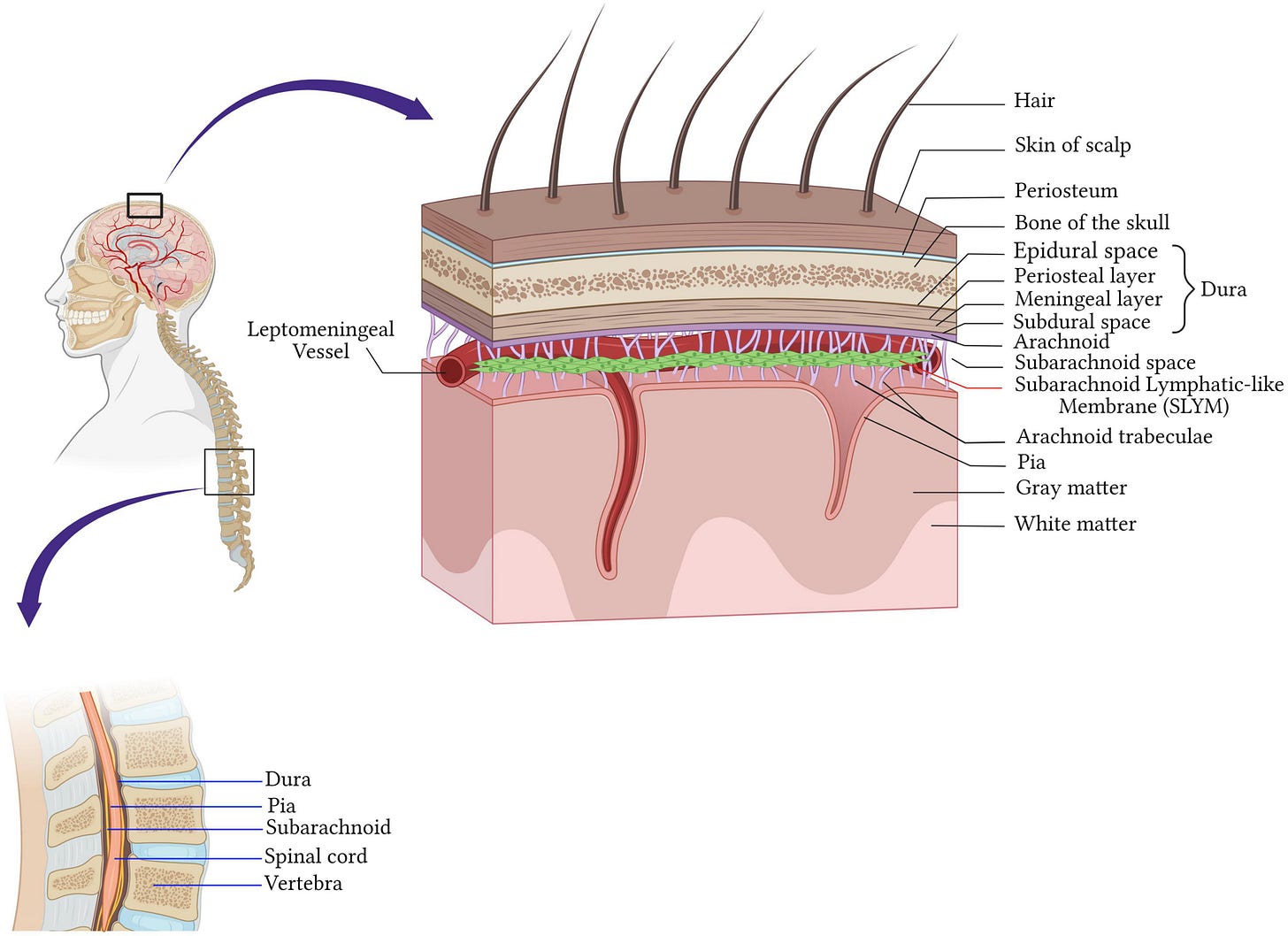
T-regs cells reside in the meninges encasing the brain and spinal cord. In mice, their immune system uses the meninges to communicate with distant neurons that detect skin sensations. When female mice were deprived of these menigeal T-regs cells, they became more sensitive to pain, while male mice did not.
Editor’s summary
Regulatory T (Treg) cells play a well-defined role in restraining inflammatory immune responses. Midavaine et al. found that depleting Treg cells specifically localized to the meninges of the central nervous system (mTreg cells) increased the responses of female, but not male, mice to mechanical pain stimuli. These mTreg cells were a source of enkephalin, an endogenous opioid peptide, within the cerebrospinal fluid. In the context of nerve injury, the enkephalin associated with mTreg cells could decrease pain sensing by activating the δ-opioid receptor expressed by a subset of nociceptive neurons involved in mechanical pain sensing. Injecting the cytokine interleukin-2 (IL-2) into the spinal fluid increased mTreg cell numbers and decreased mechanical pain sensing in female mice after nerve injury. The analgesic effect of IL-2 in female mice could be prevented by blocking female sex hormones. —Ed. Sarah H. Ross
Abstract
T cells have emerged as orchestrators of pain amplification, but the mechanism by which T cells control pain processing is unresolved. We found that regulatory T cells (Treg cells) could inhibit nociception through a mechanism that was not dependent on their ability to regulate immune activation and tissue repair. Site-specific depletion or expansion of meningeal Treg cells (mTreg cells) in mice led to female-specific and sex hormone–dependent modulation of mechanical sensitivity. Specifically, mTreg cells produced the endogenous opioid enkephalin that exerted an antinociceptive action through the delta opioid receptor expressed by MrgprD+ sensory neurons. Although enkephalin restrains nociceptive processing, it was dispensable for Treg cell–mediated immunosuppression. Thus, our findings uncovered a sexually dimorphic immunological circuit that restrains nociception, establishing Treg cells as sentinels of pain homeostasis. - É Midavaine, et al.
[Estrogen and progesterone were prompting the cells to churn out painkilling enkephalin. Is this a sex-dependent adaption to manage childbirth pain? Is this yet another reason for hormone replacement therapy in menopause?]
For further interest, another past newsletter discusses the protection that progesterone provides to the brain:
Progesterone provides neuroprotection from Parkinson's progression
My past newsletter reported studies of estradiol healing neural injuries:
“All these studies showing benefit of P4 exposure in the adult with neuronal injuries, are very encouraging. I wonder, however, if the very high levels of P4 in pregnancy are actually a protection evolved for the neonatal brain, especially for childbirth and any associated episodes of anoxia. It is already in use for prevention of preterm delivery.
Mother Nature’s wonders never cease to amaze me.”
REFERENCES
CJ Saldanha, et al. Induced Synthesis of Oestrogens by Glia in the Songbird Brain. 2013. Steroids and the Nervous System: the 7th International Steroids and the Nervous System Meeting, Turin, Italy, February, 2013. Volume 25, Issue 11. Pages 1032-1038 https://doi.org/10.1111/jne.12067
AL Pedersen, et al. Centrally Synthesized Estradiol Is a Potent Anti-Inflammatory in the Injured Zebra Finch Brain, Endocrinology, Volume 157, Issue 5, 1 May 2016, Pages 2041–2051, https://doi.org/10.1210/en.2015-1991
É Midavaine, et al. Meningeal regulatory T cells inhibit nociception in female mice. Science (2025). DOI: 10.1126/science.adq6531. www.science.org/doi/10.1126/science.adq6531








Gonadal steroids are pivotal in calibrating female T-cell responses, with broad ramifications for treating autoimmune, neurological, and endocrine disorders. The need persists for sex-specific biomedical research to address historical biases and fully harness therapeutic applications.